Dr Kamarjit Singh Mangat is consultant, department of diagnostic imaging, at the National University Hospital in Singapore. He is the author of the article “Improved Accuracy of Percutaneous Biopsy Using ‘Cross and Push’ Technique for Patients Suspected with Malignant Biliary Strictures.” that was published in the August 2015 issue of CardioVascular and Interventional Radiology (CVIR).
Remco van der Meel (global product manager, Interventional Radiology) recently spoke with Dr Mangat.
Remco: Which biliary biopsy techniques were you using before you began using transluminal forceps biopsy, and what were your success rates?
Dr Mangat: Previously we made a clinico-radiological diagnosis for suspected cholangiocarcinomas that were non–mass-forming. There was no reliable way of taking a targeted biopsy percutaneously. In some cases, we did try a brush biopsy, but yield was very low. We did not believe the negative result for malignancy and continued to treat the patient as having a presumed cholangiocarcinoma. From what we know now, in over 20% of cases we were wrong to presume cholangiocarcinoma in this non–mass-forming type of tumour.
Sometimes we would also send the bile for cytology, but again the yield was very low, and we did not believe the negative test results.
From memory, the positive yield for both of these methods was much less than 30%.
Remco: When did you start thinking about performing transluminal biliary forceps biopsy and what were your initial experiences with it?
Dr Mangat: I first tried the Cook forceps in 2005. My initial results achieved approximately 50% accuracy in the first 14 cases, but on closer analysis of the data at a certain point, I noted that when I had used a modified “cross and push” technique I always had a true positive result.
Remco: Could you please tell us more about the benefits of the modified “cross and push” technique?
Dr Mangat: Based on my initial experience described above, I started using the “cross and push” technique for all cases and found the results to be very favourable. The “cross and push” method ensures that you get a good sample of tissue from the central part of the tumour, hence the high accuracy rate.
Remco: What was the effect of this modified technique on your biopsy accuracy?
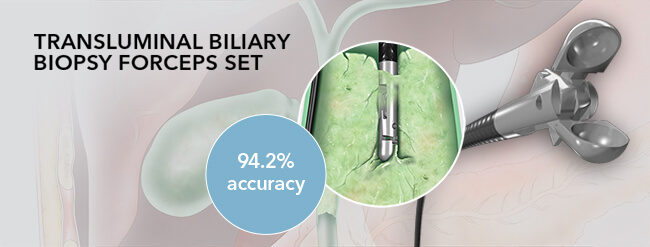
Dr Mangat: Using the modified technique, we found a massively improved accuracy rate. As we have documented in the published paper in CVIR, the accuracy rate improved to 94.2%
Remco: What outcomes of the study were surprising to you?
Dr Mangat: The most surprising finding was that, based on the original clinico-radiological methods, 1 in 5 patients was misdiagnosed. These patients actually turned out to have a benign pathology or a different malignancy altogether.
Remco: How did this finding change the way in which this cohort of patients is diagnosed?
Dr Mangat: Clearly a clinico-radiological diagnosis of a cholangiocarcinoma that is non–mass-forming is flawed, and a large number of patients were getting the wrong therapy based on the treatment being commenced without tissue diagnosis. This was in the setting of a large, tertiary-level liver unit. Prior to my documented “cross and push” technique using the Transluminal Biliary Biopsy Forceps Set, there was no reliable method of obtaining tissue from a biliary stricture. Thus, it became unacceptable to treat based on clinico-radiological testing alone.
Remco: What would you recommend to other biliary interventionists?
Dr Mangat: As there is now a documented and reliable method of sampling biliary strictures, and a clinico-radiological diagnosis is far from accurate, I would argue that it is mandatory to try to obtain a tissue sample for accurate treatment planning.
Dr Mangat is a paid consultant of Cook Medical.